Eli Lilly’s New Obesity Drug Shows Promise
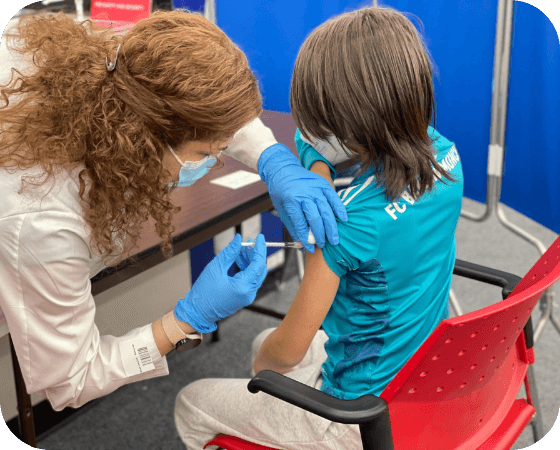
A new obesity drug from Eli Lilly helped patients lose 24% of their weight, according to phase 2 clinical trial results posted this week. Known as retatrutide, the drug is a weekly injection that imitates certain digestive hormones that help patients feel “full” and thus decreases their appetite. The clinical trial included 338 adults who were obese or overweight and had either received retatrutide injection or a placebo treatment. The results suggest retatrutide could be more effective than Mounjaro (tirzepatide), another Lilly drug that led to 21% weight loss in trials. The company is currently requiring patients participate in a phase 3 clinical trial.
CDC: Overdose Deaths from Xylazine-Laced Fentanyl on the Rise
Overdose deaths from fentanyl combined with xylazine increased by 276% between January 2019 and June 2022, according to data from the Centers for Disease Control and Prevention (CDC). However, CDC noted that the timing and scale of increase in detection of xylazine overdoses might be due to both increased frequency of testing and increased presence in the drug supply. Known as “tranq,” xylazine is an easily obtainable veterinary drug that used as a sedative and pain reliever. In recent years, drug dealers have been cutting fentanyl with xyzaline to extend a user’s high. In April 2023, the White House Office of National Drug Control Policy designated fentanyl combined with xylazine as an emerging threat.
CMS Proposes Pay Increase for Dialysis Providers
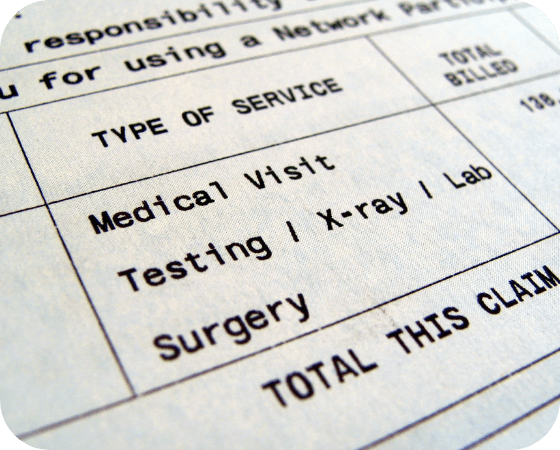
Dialysis providers could get a 1.6% payment bump from Medicare next year, according to a proposed rule for the end-stage renal disease (ESRD) Prospective Payment System (PPS). The rule contains a number of proposals related to ESRD payment policies, including a request for information (RFI) on the potential creation of a new payment adjustment that would increase payment to geographically isolated ESRD facilities. The rule also proposes a requirement on reporting of “time on machine” data, which is the the amount of time that a beneficiary spends receiving an in-center dialysis treatment. Stakeholders have until August 25, 2023 to comment on the proposed rule.
KFF: 1.5M Have Lost Medicaid Coverage since April
1.5 million people have lost Medicaid coverage in 25 states and the District of Columbia since the disenrollment process began in April, according to data from the Kaiser Family Foundation (KFF). Many states have yet to begin the disenrollment process in earnest, and KFF projects that up to 17 million people could lose their coverage. Additionally, 73% of disenrollments are due to technical reasons, such as a state Medicaid office being unable to contact an enrollee or a failure to verify income. The federal government’s options for addressing the coverage losses are limited, given that states are largely responsible for administering the program. However, the Department of Health and Human Services (HHS) did provide new flexibilities for states earlier this month intended to address disenrollment, such as allowing managed care firms to complete Medicaid renewal forms for an enrollee.
ICYMI: First-Ever Thai Festival Comes to National Mall
For the first time ever, the Thai Embassy is hosting a festival on the National Mall to celebrate 190 years of diplomatic relations between Thailand and the US. Visitors can sample various food vendors and enjoy cultural activities including Muay Thai demonstrations, Thai massages, and dance lessons. The festival is scheduled for Sunday, July 2.