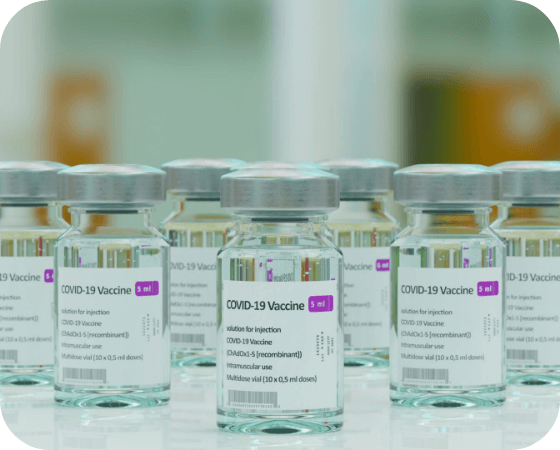
FDA Approves New Weight Loss Drug from Eli Lilly
On Wednesday, the Food and Drug Administration (FDA) approved Eli Lilly’s diabetes drug tirzepatide for chronic weight management as public health undergoes a revolution in the treatment of weight loss. Also known by its commercial name, Zepbound, the drug will be available to adults who are obese or overweight with at least one weight-related condition like high blood pressure. Zepbound is the latest in new generation appetite-suppressing obesity drugs, following Novo Nordisk’s Ozempic in 2017 and Wegovy in 2021. Eli Lilly estimates that Zepbound will be available in the US by the end of 2023 at a list price of $1,059.87.
SFC Advances Bill to Lessen Impact of Medicare Payment Cuts
Next year’s 3.4% cut to the Medicare Physician Fee Schedule (PFS) would be offset by 1.25% for one year, according to legislation unanimously advanced by the Senate Finance Committee on Wednesday. Known as the Better Mental Health Care, Lower-Cost Drugs, and Extenders Act, the bipartisan health care package contains other provisions to boost access to mental health and substance use disorder services for people enrolled in Medicare or Medicaid, address high drug costs for Medicare Part D beneficiaries, increase transparency around pharmacy benefit managers (PBMs), and other items. It is not yet clear when this package will advance through the Senate or be married up with similar legislation in the House.
CDC: Newborn Syphilis Cases Reach 30-Year High
Cases of congenital syphilis in the US reached a 3-decade height of 3,761 cases in 2022, according to new data from the Centers for Disease Control and Prevention (CDC). While syphilis cases rose among all racial and ethnic groups, the CDC noted that infants born to Black, Hispanic, or American Indian/Alaska Native mothers were up to 8 times more likely to have newborn syphilis than infants born to white mothers. The jump in cases comes amid a broader increase in sexually transmitted infections (STIs) nationwide, which public health experts attribute to a lack of access to testing and years of underinvestment in public health. The data is additionally worrying since the only recommended treatment for syphilis in pregnant people is in short supply.
Manchin Says He Won’t Seek Reelection in 2024
Sen. Joe Manchin (D-WV) announced on Thursday that he won’t be seeking reelection next year, marking the end of a 14-year stint in the US Senate. As next steps, the former West Virginia governor said he’ll be traveling the country to see if there’s interest in a “movement to mobilize the middle,” sparking concerns among Democrats that Manchin could seek a third party or independent bid for the White House in 2024. Manchin’s retirement increases the already decent odds of the GOP retaking the Senate in next year’s elections due to the state’s strong Republican bend. The centrist senator has been a key bipartisan swing vote for much of his Senate career, especially regarding President Joe Biden’s major legislative accomplishments like the American Rescue Plan Act and the Inflation Reduction Act.
ICYMI: Interactive White House Museum Coming to Downtown DC
The White House Historical Society has announced plans for a 33,000-square foot interactive museum – just a block away from the actual White House. Dubbed “The People’s House: A White House Experience,” the museum will feature recreations and replicas of the Rose Garden and the Oval Office, along with various galleries and media to give visitors a sense of what it was like to be in the Executive Mansion at different points in history. The museum is set to open in fall 2024.