AMA Downplays Importance of BMI
Physicians should deemphasize the use of body mass index (BMI) when assessing a patient’s health and obesity, according to a new policy statement from the American Medical Association (AMA). The policy was born from an AMA report that found BMI to be a flawed way to measure body fat in multiple groups because it does not account for differences across “racial/ethnic groups, sexes, genders, and age-span.” BMI was initially determined by a Belgian mathematician in the 19th century who only analyzed White non-Hispanic individuals. While the AMA acknowledges that BMI is strongly tied to the amount of fat mass in the general population, the measure becomes less relevant when applied to individuals.
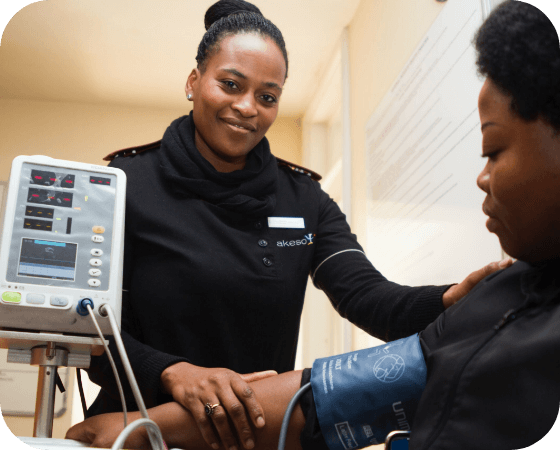
USPSTF Recommends Anxiety Screening for All Adults
Most adults should be screened for anxiety and depression even in the absence of symptoms, according to two final recommendations from the US Preventatives Services Task Force (USPSTF). In one recommendation statement, USPSTF said that all adults should be screened for major depressive disorder, including those who are pregnant, postpartum, and age 65 and older. In another recommendation statement, USPSTF said adults under age 65 should be screened for anxiety. However, USPSTF declined to recommend screening adults 65 and older for anxiety due to insufficient evidence. The new recommendations come amid a rise in adults reporting symptoms consistent with anxiety and depression since the start of the COVID-19 pandemic.
Mandy Cohen Tapped to Lead CDC
President Joe Biden announced his intent to appoint Mandy Cohen, MD, MPH as director of the Centers for Disease Control and Prevention (CDC). Cohen will begin as soon as outgoing CDC Director Rochelle Walensky, MD officially steps down on June 30, since the position won’t require Senate confirmation until January 2025. Currently CEO of Aledade Health Care Solutions, Cohen previously served as Secretary of Health in North Carolina and deputy director of the Center for Medicare and Medicaid Innovation. Biden’s announcement has drawn praise from health care stakeholders across the nation.
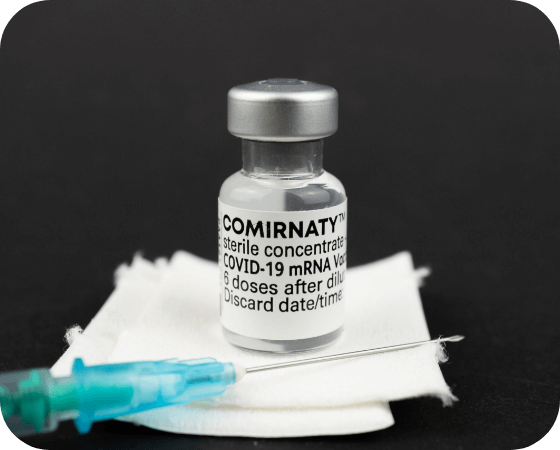
CDC Recommends RSV Vaccines for Older Adults
A CDC advisory panel voted 9-5 to recommend two respiratory syncytial virus (RSV) vaccines for adults ages 65 and older, from drug manufacturers Pfizer and GSK. Thirteen committee members, with a single abstention, also voted to recommend the vaccines for adults ages 60 to 64 based on individual risk factors and in consultation with a physician. While RSV is generally mild for most healthy adults, up to 10,000 people ages 65 and older die from RSV each year. CDC Director Rochelle Walensky is expected to endorse the vaccines soon, which is the last hurdle the vaccines must clear become they can become available to the public. Drug manufacturers and pharmacies have pledged to make the vaccines available to older adults by late fall, just in time for the winter respiratory virus season.
ICYMI: Smithsonian Folklife Festival Returns
Visitors to the nation’s capital will have another fun outdoor entertainment option when the Smithsonian Folklife Festival returns next weekend. The festival, which runs from June 29 to July 9, features participants and events from all 50 states and over 100 countries. Key programs this year include events honoring living religions in the US, the programming on culture of the Ozarks, and activities celebrating the music and food of Ukraine. Volunteers are encouraged to sign up and participate.